07 October 2020
Media release
Novel drug in development to inhibit acute inflammation
Researchers at the Baker Institute and the University of Melbourne are taking the next steps in developing a new anti-inflammatory drug that could lessen the damage from heart attacks, extend the viability of transplanted organs, help treat autoimmune diseases such as multiple sclerosis, and even reduce fatal complications from viruses like COVID-19.
The collaborative drug discovery project recently received a $200,000 boost, thanks to seed funding from the new Baker Department of Cardiometabolic Health at the University of Melbourne’s medical school, and work will now begin testing a novel drug class targeting the ‘C-reactive protein’, the best marker of acute inflammation in the body.
The project joins the teams of chief investigators Professor Karlheinz Peter, cardiologist and Deputy Director at the Baker Institute, and Professor Michael Parker, structural biologist and Director of the University of Melbourne’s Bio21 Institute.
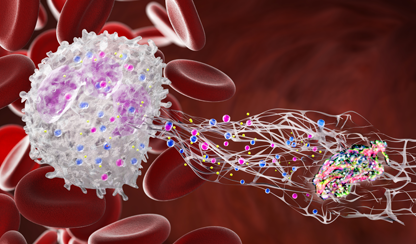
Professor Peter said they were working together on a drug to directly target the body’s inflammatory overreaction, when its immune system gets tipped into overdrive and starts to indiscriminately attack individual organs or even the whole body.
“An overshooting of the body’s inflammatory response causes some of Australia’s most common and debilitating health conditions, including atherosclerosis — the inflammation of arteries that can lead to heart attack and stroke — sepsis, multiple sclerosis, arthritis, and viral infections such as COVID-19,” Professor Peter said.
The project leverages the Baker Institute’s expertise in vascular biology alongside Bio21’s ability to investigate and visualise the 3D structures of medically important proteins using X-ray crystallography and other cutting-edge technologies. Professor Parker’s lab uses these structures to discover and develop much-needed new drugs.
Both teams have already spent significant time collaborating to characterise the C-reactive protein molecule and better understand its structure and pro-inflammatory function.
Professor Parker’s team will now identify possible drug candidates using a computational approach that searches through an in silico library consisting of thousands of drugs available for human application, as well as drug-like compounds.
Each compound will be ‘computationally docked’ into surface pockets of the C-reactive protein structure and the most promising compounds will be tested to determine the best drug candidate.
“Ultimately we want to find which of these drug compounds will fit most tightly into the C-reactive protein’s pockets and by doing so inhibit inflammation,” Professor Parker said.
“We already have some pilot data to narrow down the families of drug-like compounds that may work best. But they need optimisation to find the specific drug that will block the C-reactive protein most effectively, so patients only need to take the smallest dose.”
Testing will include experiments to see if damage from heart attacks can be lessened when the drug is administered; and past experiments with the drug-like compounds on rats showed that they could extend the life of animals with a limb transplant.
Professor Peter said a successful drug could even be used to address the health crisis currently at the top of global consciousness.
“When you have any sort of virus, the liver produces lots of this C-reactive protein, sometimes leading to a 1000-fold increase in the body. And we’ve seen with COVID-19 patients, when this protein marker is raised your chance of dying is sky high,” he said.
“So this is a nice example of how an anti-inflammatory drug could be used in the many different diseases that all have overshooting inflammatory reactions in common.
“It could also reduce the amount of muscle lost in a heart attack, address the inflammation of joints that causes arthritis, and potentially reduce the progression of multiple sclerosis and other diseases where the immune system is overacting and fighting against the body.”
Though Professor Parker said it may be several years before a drug hits the shelves.
“While the ultimate aim of our project is to have a drug on the market, drug development is costly and a lengthy process to ensure efficacy and safety in human patients,” he said.
“We expect that by continuing this significant collaboration, and by elevating that work through the new Baker Department of Cardiometabolic Health at the Melbourne Medical School, we will attract the further funding we need to get a highly promising drug to market.”
This project is a collaboration between Professor Karlheinz Peter, Dr James McFadyen, Dr Guy Krippner and Professor Geoff Pietersz from the Baker Heart and Diabetes Institute, and Professor Michael Parker, Dr Tracy Nero, Dr Steffi Shing Cheung and Dr Craig Morton from the Bio21 Institute.
For further information or to organise interviews please contact:
Tracey Ellis
T: 03 8532 1514
M: 0433 781 972
E: tracey.ellis@baker.edu.au